Objective diagnostic tests
This section explains the tests you can perform to provide objective evidence that your patient has asthma.
In asthma, chest symptoms are accompanied by variable narrowing and or inflammation of the airways which can be measured using breathing tests.
The main way of detecting inflammation is through blood and FeNO testing which measures inflammation caused by eosinophils.
Remember that symptoms, airway narrowing and inflammation in asthma can vary a lot over time and sometimes this means tests can be normal if they’re done when a person doesn’t have symptoms. Take into account whether the patient was symptomatic and what medication they had taken when interpreting results.
Blood testing
Blood testing
The inflammatory cells of the airway in asthma are eosinophils, which can be detected in your patient’s blood.
Fractional Exhaled Nitric Oxide (FeNO)
FeNO testing measures nitric oxide, an inflammatory biomarker which is produced in the lungs and detected in exhaled breath.
Eosinophilic inflammation is the most common type of inflammation seen in asthma and it usually responds very well to inhaled corticosteroids.
The FeNO level will go up if there is untreated eosinophilic inflammation in the airways and this can help you to decide whether someone has asthma or not. It can also be used to tell whether someone with asthma is on enough of the right medicines to dampen down the eosinophilic inflammation in their airways.
Interpreting FeNO results
A low FeNO (less than 25ppb) indicates minimal eosinophilic inflammation.
A high FeNO (more than 50ppb) suggests significant eosinophilic inflammation.
Intermediate FeNO levels (25 – 40ppb) is inconclusive on its own so you will need to consider changes from previous readings, then look at your patient’s history and other tests to make a decision.
It’s important to remember that only around 50% of all cases of asthma have eosinophilic features. This means that a positive FeNO test increases the probability of asthma but a negative test does not exclude a diagnosis of asthma, because that patient might not have eosinophilic type asthma.
FeNO results can be affected by several factors. High FeNO can be due to allergic rhinitis or nitrate rich foods such as green leafy vegetables (for example, celery, leek, beetroot, lettuce and spinach).
Exercise may also raise FeNO levels, whereas caffeine, alcohol, and tobacco may decrease FeNO levels.
An information video and leaflet can be sent to your patient advising them of foods and activities to avoid ahead of their appointment.
FeNO can also be used to help patients understand and visualise the airway inflammation linked to asthma diagnosis.
Repeating FeNO testing after treatment has been started (for example, after a trial of treatment) can show your patient that it is effective and motivate them to continue. A persistently high FeNO level can also highlight problems with inhaler technique or your patient’s ability to stick with their treatment regime.
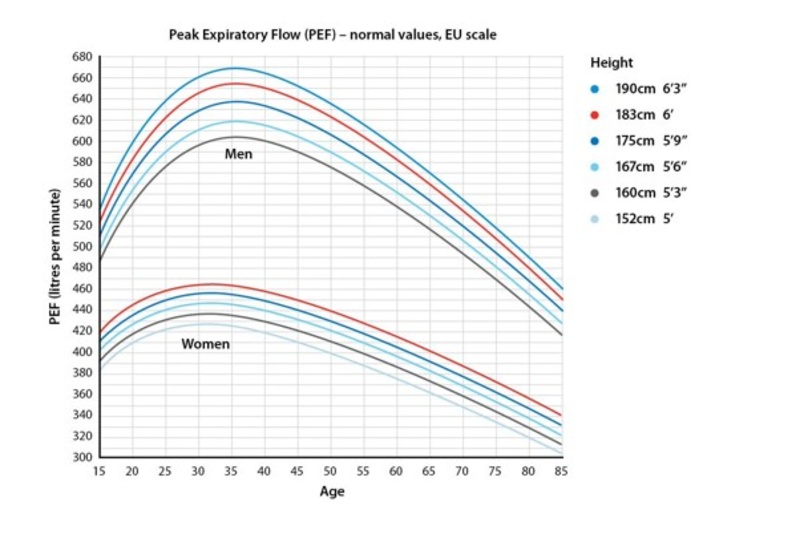
Peak expiratory flow
Peak flow measures the highest airflow rate in litres per minute during forceful exhalation after taking in a full breath.
It is useful in demonstrating variability of airflow obstruction or limitation. It can also be used to demonstrate reversibility if spirometry is not available.
PEF is used for the diagnosis, self-management and assessment of severity of asthma attacks.
There are predicted values for peak flow, but they should only be used as a guide. This is because peak flow will vary from person to person.
It’s important that patients know what their usual peak flow is, as this measurement can be used to guide their self-management plan and help them to notice if their asthma is getting worse.
Your patient should use the same meter each time PEF is measured, as readings between meters can vary.

Good technique is essential to ensure accurate peak flow readings. Use the video below to guide your patient.
0:00
Hi I'm Naomi. I'm a respiratory nurse specialist at Asthma + Lung UK.
0:05
I'm going to tell you how to use a peak flow meter. When you first
0:10
get a peak flow meter, ask your GP, asthma nurse or pharmacist
0:14
to show you how to use it and how to take a reading.
0:17
If you're checking your peak flow at home,
0:20
you need to take your peak flow at least twice a day, every day
0:24
to get a useful pattern of results.
0:26
Try to check it at the same time every morning and every evening.
0:30
You need to use your best effort every time you blow into the meter
0:34
so you're comparing like with like and you should use the same peak
0:37
flow meter every time.
0:39
Take these steps to make sure you use your peak flow meter correctly.
0:43
Pull the counter, the red arrow, back as far as it will go,
0:48
to the top, near the mouthpiece. Stand or sit upright.
0:53
Choose what's most comfortable for you and always do it that way.
0:57
Then take the deepest breath you can and make sure your mouth makes
1:02
a tight seal around the mouthpiece. Then blow as hard and as fast as
1:07
you possibly can into the meter, like this.
1:14
Write down your score which is the number next to the pointer.
1:18
Do this three times in a row with a short rest in between
1:22
so that you get three scores. All three readings should be
1:26
roughly the same but don't worry too much if they vary.
1:30
Use the highest of these scores to fill in your peak flow diary.
1:34
If you have any questions about using your peak flow meter
1:37
speak to your doctor, nurse or pharmacist.
1:40
You can also call our helpline.
Peak flow diaries
PEF in patients with asthma is usually lower in the morning and higher in the evening. This is called diurnal variation.
For accurate results the PEF should be recorded at least twice a day, on waking and ideally around 4pm when peak flow tends to ‘peak’. The patient should perform at least 3 blows and record the highest number . The diary should be kept for 2-4 weeks.
Click here to download peak flow diaries
Diurnal variation of 20% is suggestive of asthma.
Click here to use our calculator to work out your patient’s percentage
Demonstrating reversibility with PEF
PEF can be used to demonstrate reversibility if spirometry is not available.
You will need to ensure that your patient is prescribed a salbutamol inhaler and spacer prior to their appointment.
Record a pre bronchodilator PEF (best of 3 blows)
Give a dose of salbutamol (400 μg via an inhaler and spacer device).
After 15 minutes, record a post bronchodilator PEF (best of 3 blows)
Variation of 20% is suggestive of asthma.
To calculate:

Spirometry
Spirometry is an objective diagnostic test which must be quality assured. It should only be performed and technically reported by an HCP who has undergone appropriate training.
The ARTP Spirometry National Register is a list of HCPs who have completed the ARTP Spirometry Certification. Joining the National Register is not mandatory but it ensures that all HCPs have their skills assessed and are certified as competent.
For advice and support on choosing the right training for you, please see our training and development page.
Spirometry with reversibility is the objective test for asthma.
A patient with untreated asthma may have bronchoconstriction in their airways and an obstructive pattern on spirometry: their FEV1/FVC will be less than 70%, or their Z score lower than -1.645.
Reversibility testing relieves this bronchoconstriction. You can diagnose asthma if the FEV1 increase is 12% or more and 200 ml or more from the pre-bronchodilator measurement (or if the FEV1 increase is 10% or more of the predicted normal FEV1)
Remember: if your patient is not symptomatic on the day when they are tested, their spirometry may be normal. This doesn't mean they don't have asthma!
This is why it can be a good idea to use peak flow measurements as well as spirometry, to capture variability in symptoms.